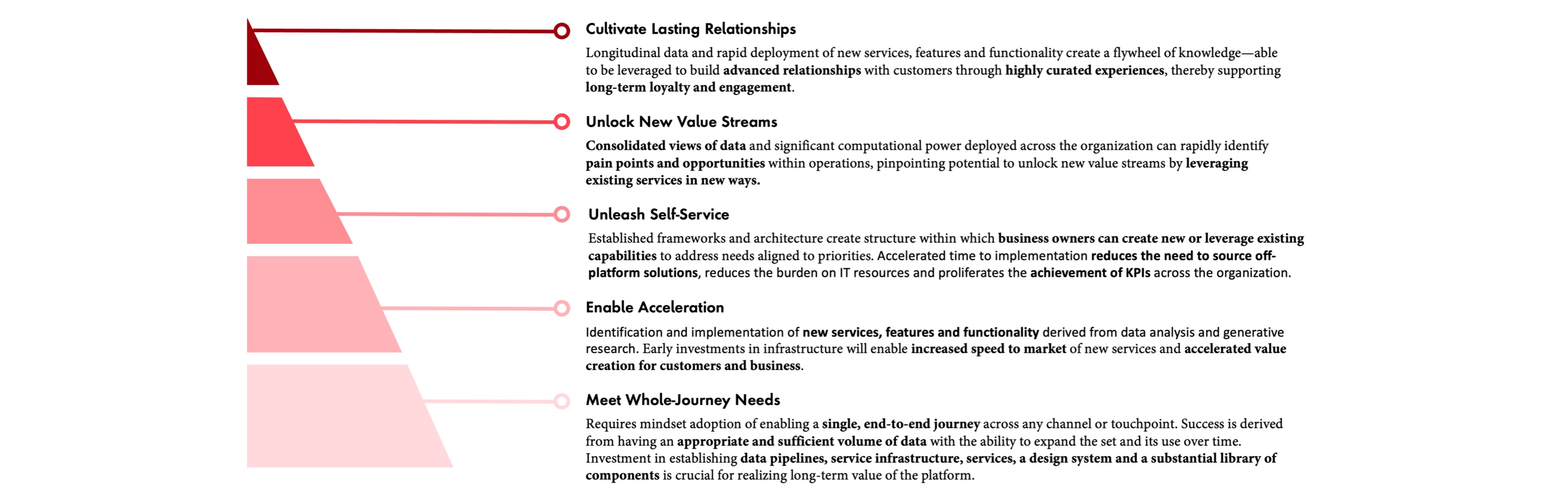
However, it’s more than just applying the right architecture principles. Modern platforms are built in a very different way compared to those of the past. Consider how skyscrapers are built. A developer will hire an architect and engineers to come up with the building design, which may be, for example, 18 stories high, with x amount of commercial space, y number of apartments and z amount of car parking. The elevator fire escape shafts will be built according to regulations, the ventilation systems will be placed on the roof and the plumbing will be structured per the specifications. It’s designed, then built, then used—18 stories, $450 million, job done. That’s how old platforms were built. New platforms are designed differently. The architect and engineers will start by focusing on the services needed (such as ventilation, plumbing and floor-to-floor access), and build a few floors. Then more floors will be built as needed. The services will be standardized, making it seamless to “move” between skyscrapers. The point is, it’s a completely different way of building things that isn’t about building a fixed system that becomes legacy technology, but rather something that is far “lighter,” more flexible and evolves over time.
The frontline challenges: keeping it real
It’s one thing to write about the future, about “what” must be built, but truth be told, the real innovations are around “how” to get there. It's worth reflecting on current state issues for healthcare organizations—issues that make digital transformation in healthcare particularly challenging. Of course, the specific circumstances for each healthcare organization have unique nuances, but generally, there are four key drivers consistently seen across healthcare organizations that have left many leaders feeling unsure of how to move forward.
Risk of disruption to daily operations
Whether it is reviewing a patient’s health history, navigating clinical workflows or processing insurance claims, platforms are supporting huge swaths of activity happening every minute within healthcare organizations. Employees have learned the capabilities—and limitations—of these platforms, passing on workarounds and precautions to new colleagues. This acceptance of the status quo isn’t due to a lack of desire for change. Rather, it’s a need to ensure that the vital services being provided are not interrupted, giving way to the old adage that sometimes, it's better to deal with the devil you know than the devil you don't.
High volumes of (sensitive) data
Over 30 percent of all data in existence today is generated by the healthcare industry, and the average hospital produces an additional 137 terabytes per day. Much of this is personal health data which comes with an additional layer of security requirements and government regulations. The management and movement of this data is an enormous task that few off-the-shelf platforms are capable of managing effectively and securely, not to mention the potential risks associated with migration. Furthermore, organizations are faced with the crucial and complicated task of thoughtfully constructing and carefully managing data privacy and consent across their organizations.
Lack of standardized structures
When each EHR is implemented, it severs ties with its mother platform and becomes a bespoke instance with its own qualities, quirks and capabilities. This can negatively impact the usability of the data it’s capable of sharing. Adherence to Fast Healthcare Interoperability Resources (FHIR) and Health Level Seven (HL7) only ensures information is able to be transferred between organizations. The Sequoia Project, recognized by the Office of the National Coordinator for Health Information Technology (ONC) as the coordinating entity for TEFCA, highlights the issue. According to The Sequoia Project, it’s one thing to get health data to the right place at the right time; it’s quite another to make sure that data is complete and useful. Without standard structures and taxonomies for all kinds of data (clinical, educational, diagnostic), there will continue to be high friction between and within healthcare organizations, inhibiting the instigation of a true platform ecosystem.
Unclear or delayed ROI
With significant capital needed to transform such large and vital platforms, organizations rightly expect to be able to quantify the impact of their investments. However, the more noteworthy results, such as lower cost to serve, higher patient satisfaction and improved health outcomes, often take a long time to be realized. Meanwhile, short-term gains like maintenance costs, increased productivity and more consumer data capture points can be overshadowed by the high degree of short-term investments and change management required to get there.
Planning the revolution
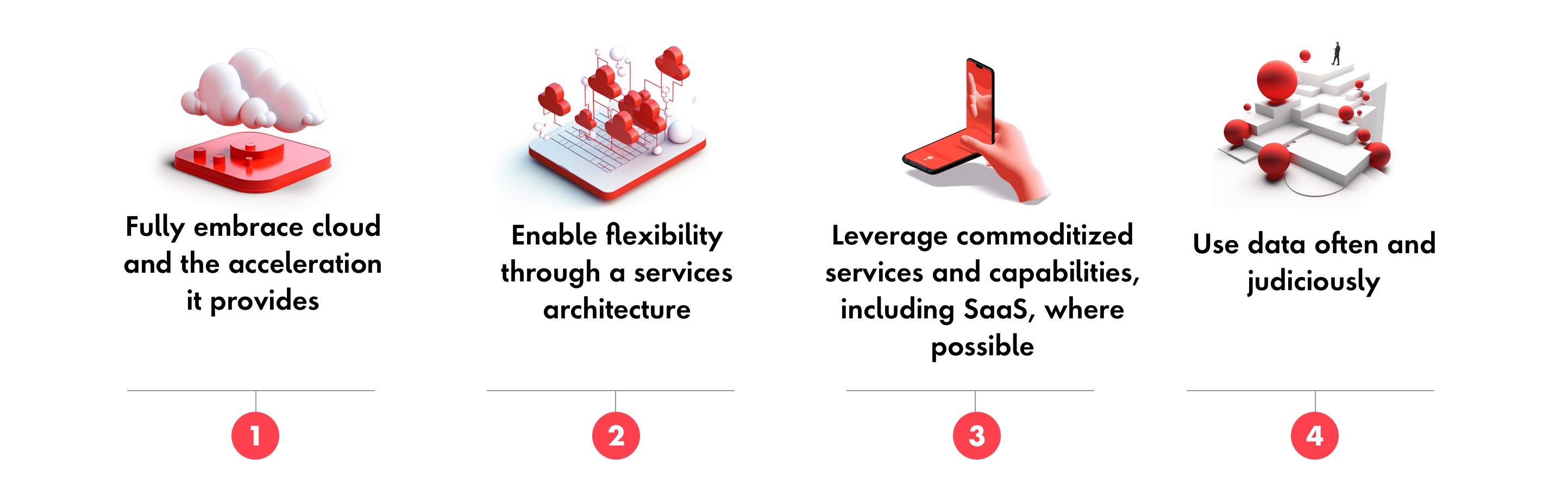
To develop the next generation of platforms, organizations must structure a two-stage plan. First, each healthcare organization needs to anchor their approach around the following four areas: